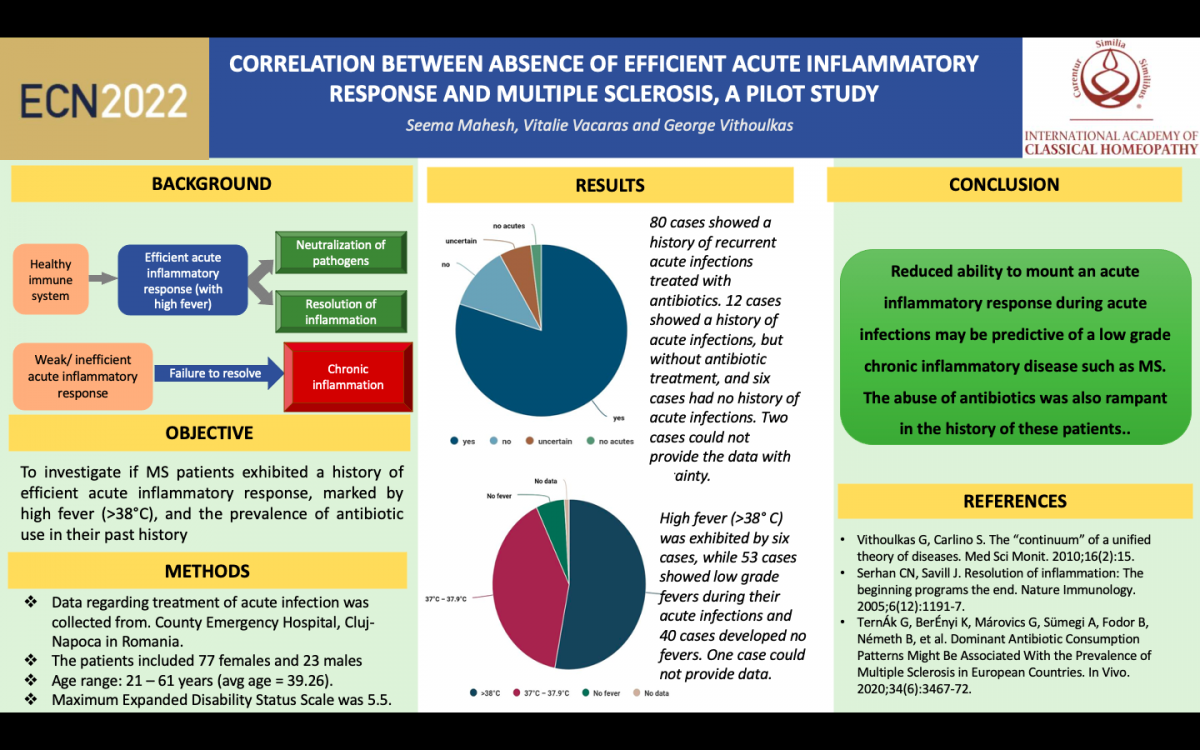
Correlation between absence of efficient acute inflammatory response and multiple sclerosis, a pilot study
(Oral Presentation – Our poster was selected as one of the best abstracts and given a video presentation opportunity – you will see the video below)
Authors: Seema Mahesh1, Vitalie Vacaras2 and George Vithoulkas3
1Centre for Classical Homeopathy, Vijayanagar Bangalore, India,
2University of Medicine and Pharmacy, Iuliu Hatieganu, Cluj-Napoca, Romania and
3University of the Aegean International Academy of Classical Homeopathy, Alonissos, Greece
Abstract topic: Emerging concepts for understanding and treating patients with neuroinflammation and neurodegeneration, with a particular focus on multiple sclerosis
Abstract:
Background: Efficient acute inflammatory response, signified by the ability to mount a high fever during common infections is the hallmark of a healthy immune system (1-4). Inability to do so eventually leads to disrupted resolution of the inflammation and the perpetuation of a low grade chronic inflammatory state (5-9). This phenomenon may be operational in the triggering of many chronic diseases including Multiple sclerosis (MS) (7, 10), and may be worsened by the abuse of antibiotics (11, 12), which further suppress the inflammatory response.
Objective: To investigate if MS patients exhibited a history of efficient acute inflammatory response, marked by high fever (>38oC), and the prevalence of antibiotic use, in their past history
Methods: We collected data from 100 consenting MS patients visiting the Department of Neurosciences, County Emergency Hospital, Cluj-Napoca in Romania, regarding the past history of treatment of acute infections. The patients included 77 females and 23 males, ranging from 21 to 61 years of age (average age of 39.26). The maximum Expanded Disability Status Scale was 5.5.
Results: Of 100 cases, 80 cases showed a history of recurrent acute infections treated with antibiotics. 12 cases showed a history of acute infections, but without antibiotic treatment and six cases had no history of acute infections. Two cases could not provide the data with certainty. High fever (>38o C) was exhibited by six cases, while 53 cases showed low grade fevers during their acute infections and 40 cases developed no fevers. One case could not provide data.
Conclusion: Reduced ability to mount an acute inflammatory response during acute infections may be predictive of a low grade chronic inflammatory disease such as MS. The abuse of antibiotics was also rampant in the history of these patients These findings need deeper scientific investigation into all the parameters involved, including the repeated treatment with antibiotics
References:
1. Evans SS, Repasky EA, Fisher DT. Fever and the thermal regulation of immunity: The immune system feels the heat. Nature Reviews Immunology. 2015;15(6):335-49.
2. Fisher DT, Vardam TD, Muhitch JB, Evans SS. Fine-tuning immune surveillance by fever-range thermal stress. Springer; 2010. p. 177-88.
3. Bhavani SV, Huang ES, Verhoef PA, Churpek MM. Novel Temperature Trajectory Subphenotypes in COVID-19. Chest: American College of Chest Physicians; 2020. p. 2436-9.
4. Cann SAH. Fever: could a cardinal sign of COVID-19 infection reduce mortality? The American Journal of the Medical Sciences. 2021.
5. Panigrahy D, Gilligan MM, Huang S, Gartung A, Cortés-Puch I, Sime PJ, et al. Inflammation resolution: a dual-pronged approach to averting cytokine storms in COVID-19? Cancer Metastasis Rev. 2020;39(2):337-40.
6. Serhan CN, Savill J. Resolution of inflammation: The beginning programs the end. Nature Immunology. 2005;6(12):1191-7.
7. Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019;25(12):1822-32.
8. Lawrence T, Gilroy DW. Chronic inflammation: a failure of resolution? Int J Exp Pathol. 2007;88(2):85-94.
9. Vithoulkas G, Carlino S. The “continuum” of a unified theory of diseases. Med Sci Monit. 2010;16(2):15.
10. Zéphir H. Progress in understanding the pathophysiology of multiple sclerosis. Revue neurologique. 2018;174(6):358-63.
11. Baldin E, Zenesini C, Antonazzo IC, Bartolomei I, Caniatti L, Costa M, et al. Antibiotic Use and Risk of Multiple Sclerosis: A Nested Case-Control Study in Emilia-Romagna Region, Italy. Neuroepidemiology. 2021;55(3):224-31.
12. TernÁk G, BerÉnyi K, MÁrovics G, SÜmegi A, Fodor B, NÉmeth B, et al. Dominant Antibiotic Consumption Patterns Might Be Associated With the Prevalence of Multiple Sclerosis in European Countries. In Vivo. 2020;34(6):3467-72.